
Cryosurgery in dermatology
- Cryosurgery is a relatively safe and simple dermatologic procedure with few contraindications and low complication rate.
- Liquid nitrogen is the most effective and most studied cryogen.
How does it work? ( mechanism of action)
- Direct injury:
- Formation of ice crystals after freezing the tissue water leading to necrosis, it requires a temperature of -20 for most tissues and -50 or lower for neoplastic lesions.
- Vascular injury:
- Damage to the vascular endothelium leading to ischemia.
- Apoptosis
- Immunlologic stimulation produced by the release of antigenic components results in cell damage
Thawing time should be at least 1.5 times longer than the freezing time for adequate cryosurgery.
Maximum damage is produced by rapid freezing and slow thawing
What are the uses of Cryosurgery in dermatology?
Benign lesions
- Acne (cryopeeling)
- Vascular lesions
- Venous lake.
- Cherry angioma.
- Capillary hemangioma
- Vascular malformations of blue rubber bleb nevus syndrome.
- Pyogenic granuloma.
- Cysts and tumors
- Milia
- Myxoid cyst
- Skin tags
- Seborrheic keratosis.
- Dermatofibroma.
- Oral mucocele.
- Sebaceous hyperplasia.
- Solar lentigo.
- Others
- Warts.
- Hypertrophic scarring and keloid.
- Rhinophyma.
- Epidermal nevi.
- Lobomycosis.
- Cutaneous horn.
- Ingrown nail.
- Molluscum contagiosum.
- Cryolipolysis.
Premalignant lesions
- Actinic keratosis.
- Bowen disease.
- Keratoacnthoma.
Malignant lesions
- Nonmelanoma skin cancers e.g SCC or BCC.
- Kaposi sarcoma.
- Lentigo maligna.
What are the complications of Cryosurgery?
- Cryotherapy pain
- Transient.
- Pain threshold is different from one patient to another.
- Topical anesthesia can be helpful for superficial treatment in children.
- Haemorrhagic blisters
- Erythema, edema.
Blister formation is not necessary for the cure of lesions such as
viral warts
- Dyspigmentation
- Hypopigmentation with deep freezing is common in dark‐skinned patients and may be permanent.( Melanocytes only require a temperature of -5°C for destruction). Perform a test in a not visible area to detect the potential of dyspigmentation.
- Post‐inflammatory hyperpigmentation with light freezing.
- For non-malignant sites, freezing for 10–15 s minimizes hypopigmentation.
- Deep freezing over the lacrimal ducts may, very rarely, lead to permanent ductal obstruction.
- Neuropathy
- Nerve damage resulting in paraesthesiae, distal anaesthesia and motor paralysis occasionally occur.
- Areas which require special caution include the pre- and post-auricular areas, lateral aspects of the fingers, lateral aspect of tongue, and ulnar fossa.
- Pseudoepitheliomatous hyperplasia: self limited.
- Nail dystrophy.
- Damage to tendons
- Alopecia
- It may occur at hair bearing areas and may be permanent.
- Freezing for 15–20 s may cause permanent hair-loss.
- Scar formation.
- Infection
- Pyogenic Granuloma
- Febrile reaction (Flu like) may occur after treatment of large or multiple lesions at one sitting, it subsided within 24-36 hrs.
- Syncope : It may due a vasovagal attack.
Before cryosurgery is performed a diagnosis must be made either by histologic or clinical and dermatoscopic diagnosis.
Contraindications
Absolute
- Cold urticaria.
- Previous history of cold induce injury at the site or limb.
- Cryoglobulinemia.
- Cold intolerance
- Cryofibrinogenemia.
- Immunosuppression.
- Poor circulation at the site or in that limb.
- Multiple myeloma.
- Raynaud disease.
- Pyoderma gangrenosum.
- Unexplained blood dyscarsia
Relative
- Prior adverse reaction to cryosurgery, such as anaphylaxis or severe cold urticaria.
- Poor circulation at the site or in that limb.
- Intake of immunosuppressive drugs
Pre-treatment Considerations
- Patient selection.
- Lesion selection
- Patient education : thorough explanation on the procedure
- Patient consent.
- Explain to the patient all the treatment options as well as the expected secondary effects, the possible complications, the postoperative care, and the time expected for final healing.
- Keratin removal will allow for a better penetration of the freezing front.
How to prepare the skin before cryosurgery?
- For hyperkeratotic lesions, curettage should be performed to allow for better and more accurate administration of liquid nitrogen.
- Cryosurgery of small lesions does not usually need intralesional anesthesia.
- Topical anesthesia may be required before cryosurgery of the large lesions.
Technique
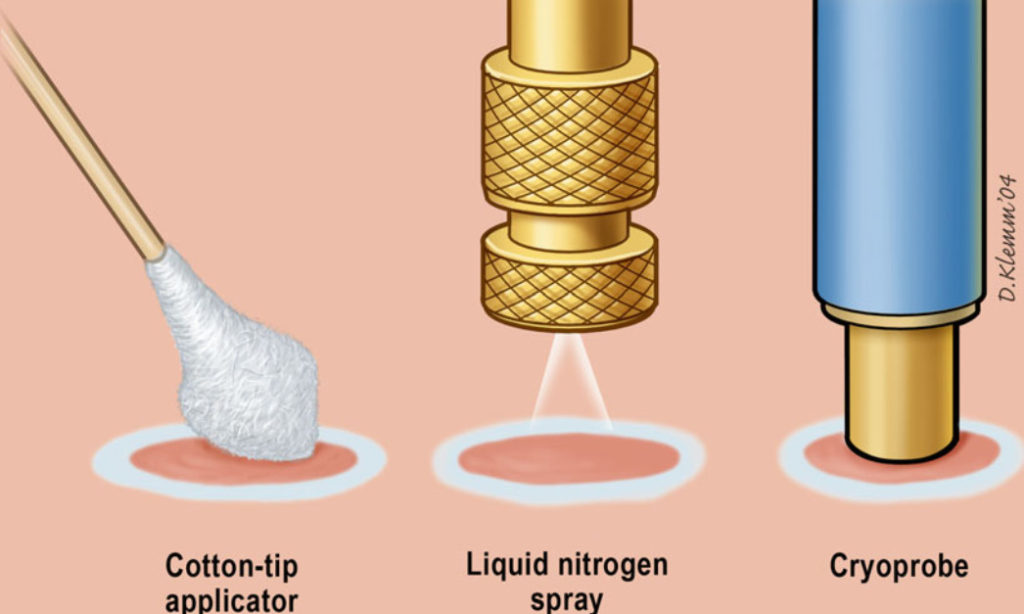
- Based on the confirmed diagnosis, determine the suitable technique (Open spray technique- contact cryotherapy(Cryoprobe) – intralesional cryotherapy).
- Paring the lesion for removal of the superficial keratin layer ( warts) or application of keratolytics like salicylic acid in 2 weeks prior to cryosurgery.
- Determine the suitable freezing time, the number of cycles and the required margin, taking into consideration the sensitivity of different cell types to cryotherapy.
- Margins for most benign lesions are 1–2 mm beyond the visible pathologic border.
- Premalignant lesions need margins of 2–3 mm, while malignant lesions require margins of 5 mm of clinically normal skin to ensure adequate removal.
Sensitivity of different cell types to cryoinjury
| Melanocytes destroyed at | -4 to -7 °C |
| Sebaceous glands and hair follicles destroyed at | -20 °C |
| Keratinocytes destroyed at | -20 to -30 °C |
| Fibroblasts destroyed at | -30 to -35 °C |
| Benign tumors destroyed at | -20 to -25 °C |
| Malignant tumors destroyed at | -50 to -60 °C |
The treatment time of 30 s usually forms epidermo-dermal separation and hemorrhagic blister but never produces scarring or keloids.
Freezing time for different skin lesions.
The freezing time is adjusted according to variables such as skin thickness, vascularity, tissue type ,site, and lesion characteristics.
Smaller flatter lesions require only 5–10 s of freezing and one cycle only. Larger thicker lesions may require longer duration of freeze up to 20 or even 30 s.
- Cryosurgery treatment of warts
- Molluscum contagiosum : 5-10 seconds
- Cutaneous horn: 10 -15 seconds, single freeze, open spray technique.
- Ingrown nail: 30 seconds, single freeze.
- Dermatofibroma:20-60 s, 1-2 cycles, 2-3 mm margin, open spray technique.
- Hypertrophic scar : 20 s, 1 cycle, 2 mm margin, open spray technique.
- Keloid : 30 s, 1-3 cycles, 2mm margin, open spray technique.
- Myxoid cyst: 20 s, 1 cycle, < 1 mm margin, open spray technique.
- Oral mucocele : 10 s, 1 cycle, < 1 mm margin, cryoprobe.
- Pyogenic granuloma: 15 s, 1 cycle, < 1 mm margin, open spray technique.
- Seborrhoeic keratoses : A single freeze time of 10-20 seconds depending on the thickness.
- Actinic keratosis : A single freeze time of 5-20 seconds is adequate for most cases, open spray technique.
- Solar lentigo : 5 s,1 cycle, < 1 mm margin, open spray technique
- Sebaceous hyperplasia : 10-15 s, 1 cycle, < 1 mm margin, cryoprobe.
- Skin tags: 5 s, 1 cycle, 1 mm margin
- Bowen’s disease : 20 – 30 single freeze, 1-2 cycle, 3 mm margin, open spray technique.
- Keratoacanthoma : 30 s, 2 cycles, 5 mm margin, open spray technique
- BCC : 60-90 s, 2-3 cycles, 5 mm margin, open spray technique
- SCC : 60-90 s, 2-3 cycles, 5 mm margin, open spray technique
- Kaposi sarcoma: 20-40, 1-2 cycles, 3 mm margin.
- Lentigo malgina: 60 s, 2 cycles,5 mm margin, open spray technique.
#Cryosurgery #Cryosurgery in dermatology