Definition and Prevalence
- Pruritus is an unpleasant sensation that causes a strong urge to scratch, negatively impacting psychological and physical well-being.
- Chronic pruritus (CP) is defined as an unpleasant sensation resulting in a need to scratch that lasts more than 6 weeks.
- It is one of the major dermatological complaints during pregnancy.
- Recent studies indicate that 18-40% of pregnant patients experience pruritus.
Associated Conditions
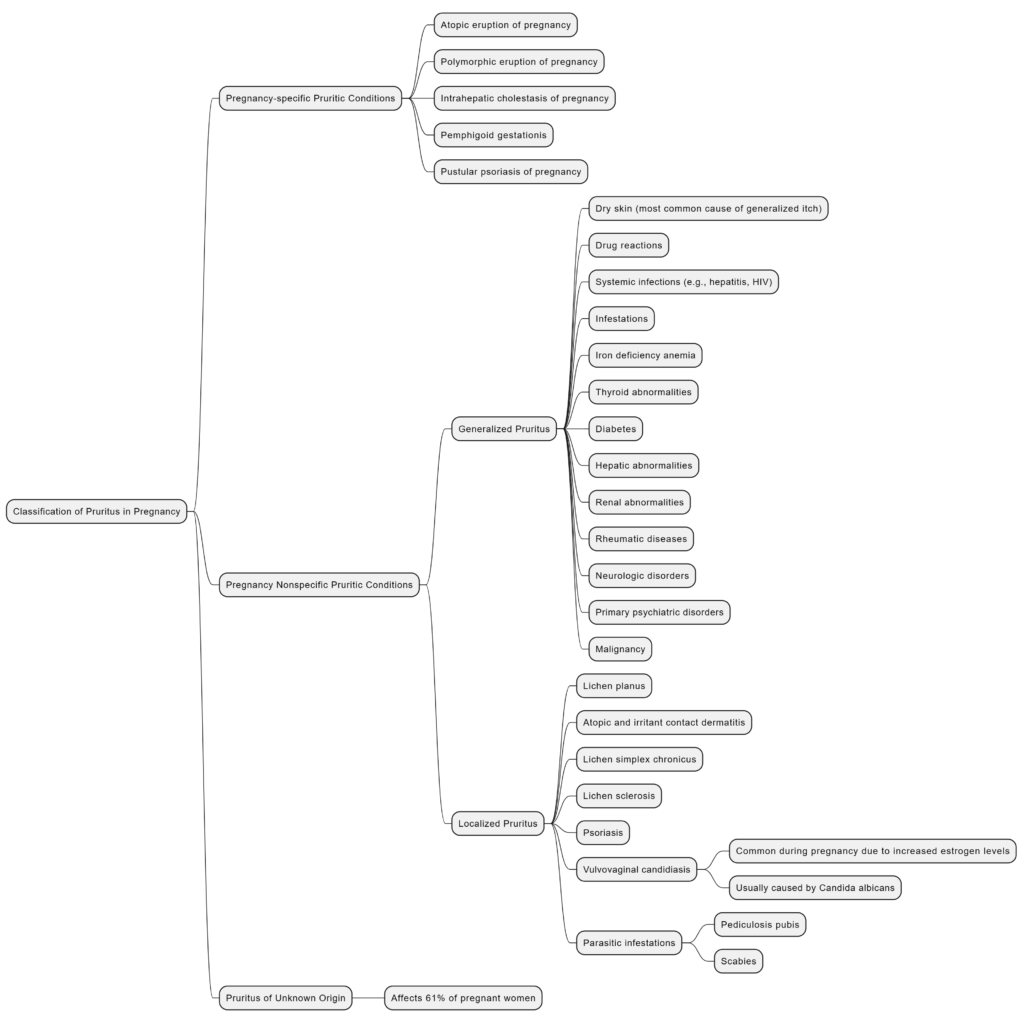
CP can be associated with pregnancy-specific conditions such as:
- Atopic eruption of pregnancy (AEP)
- Polymorphic eruption of pregnancy (PEP)
- Pemphigoid gestationis (PG)
- Intrahepatic cholestasis in pregnancy (ICP)
Pruritus may also arise from:
– Dermatoses coincidentally developing during pregnancy
– Exacerbation of preexisting dermatoses
– Physiological skin changes in pregnancy
Pregnancy-specific conditions
Atopic Eruption of Pregnancy (AEP)
Definition and Introduction
- In 2005, Ambros-Rudolph et al. introduced AEP as an umbrella term for benign pruritic disorders of pregnancy.
- AEP includes conditions previously diagnosed as eczema of pregnancy, prurigo of pregnancy, and pruritic folliculitis of pregnancy.
Epidemiology
- AEP is the most common dermatosis of pregnancy.
- AEP encompasses:
- Patients with exacerbation of preexisting atopic dermatitis (approximately 20% of cases).
- Patients experiencing skin manifestations for the first time during pregnancy.
Risk Factors
- Patients with a family history of atopic dermatitis are at increased risk of developing AEP.
- The disease is often idiopathic, occurring without a known cause.
Types of AEP
- E-type (Eczematous):
- Classical distribution of lesions.
- Eczematous eruption on the face, neck, pre-sternal region, and flexure sides.
- P-type (Prurigo):
- Presence of small, pruritic, erythematous, often grouped papules.
- Predominantly on the extensor surfaces of the extremities and the trunk.
Coexistence and Generalization:
- E and P types often coexist.
- Lesions can generalize.
- Secondary lesions include excoriations from scratching and bacterial or viral superinfection (e.g., eczema herpeticum).
Diagnostic Workup
Medical History and Examination:
- Detailed medical history.
- Comprehensive dermatological examination of the entire skin, including mucosae.
Clinical Presentation:
- Early onset of eczematous/prurigo skin lesions (before the third trimester).
- Involvement of the trunk and limbs.
- Possible atopic family or personal background.
Histopathology:
- Nonspecific and varies with clinical type and stage.
- Skin biopsy is not indicated for diagnosis but may help exclude other causes of pruritus.
Immunofluorescence:
- Direct immunofluorescence (DIF) and indirect immunofluorescence results are negative.
Laboratory Tests:
- Elevated serum immunoglobulin E (IgE) levels in about 30–70% of cases.
- The role of IgE levels as a diagnostic criterion is unclear.
Allergy Tests:
- Prick and patch tests are not recommended during pregnancy.
Treatment
Patient Education:
- Emphasis on sufficient emollient therapy as basic dermatological care.
- Various compounds were studied for their contribution to skin hydration and reduction in pruritus.
Second-line Treatment for Mild and Moderate AEP:
- Topical Glucocorticosteroids:
- Used to manage mild and moderate AEP.
- Systemic Antihistamines:
- Recommended alongside topical treatments.
- Narrowband Ultraviolet B (UVB):
- Recommended for moderate and severe AEP, especially in early pregnancy.
- Second-line Treatment for Severe AEP:
- Systemic Glucocorticosteroids:
- Short-term use for recalcitrant pruritus.
- Prednisolone dosage: 0.5–2 mg/kg/day.
- Immunosuppressive Agents:
- Considered for severe cases unresponsive to phototherapy.
- Cyclosporine or Azathioprine:
- Introduced with caution, weighing risks and benefits.
- Azathioprine may be used off-label if other therapies fail or cyclosporine is contraindicated.
Potential Future Therapy Option:
- Dupilumab:
- Anti-interleukin-4 receptor (IL-4R)-α antibody.
- Inhibits IL-4 and IL-13 signaling, affecting various immune cells.
- Promising safety profile in case reports, but more evidence needed.
- Recommended to postpone use in pregnancy until more data is available.
Prognosis and Fetal Risks
Reassurance:
- Excellent prognosis for AEP.
- Not associated with adverse fetal outcomes.
Potential Predisposition:
- Children might be predisposed to atopic eczema based on their parents’ atopic background.
- The disease may recur in subsequent pregnancies.
Polymorphic Eruption of Pregnancy (PEP)
Definition and Epidemiology
- Also known as pruritic urticarial papules and plaques of pregnancy(PUPPP).
- Benign, self-limiting pruritic inflammatory disorder.
- Incidence: 1 in 120 to 1 in 300 pregnancies.
- Typically occurs in the third trimester or immediately postpartum (about 15% of cases).
- Risk factors include:
- First pregnancy (primigravida)
- Excessive maternal weight gain
- Multiple pregnancies
Pathophysiology and Clinical Characteristics
Theories of Pathogenesis
- Skin stretching in the third trimester or over multiple pregnancies may activate dermal nerve endings, leading to pruritus.
- Possible damage to collagen fibers may induce an allergic-type response, contributing to PEP lesions.
Clinical Presentation
- Polymorphic skin lesions: highly pruritic urticarial papules coalescing into plaques.
- Small vesicles (1–2 mm) without bullae.
- Widespread non-urticated erythema, targetoid, and eczematous lesions.
- Generally spares the periumbilical region, this helps to differentiate PUPPP from PG.
- Lesions often start in the abdominal region within striae distensae and spread to thighs, buttocks, and trunk; distal extremity involvement is rare.
Diagnostic Workup
Diagnosis
- Based on clinical presentation.
- No characteristic histological or immunofluorescence findings.
- Prolonged follow-up is recommended to distinguish from pre-bullous pemphigoid gestationis (PG).
- Direct immunofluorescence (DIF) may be performed if there is clinical uncertainty to rule out pre-bullous PG.
Treatment
First-line Treatments
- Emollients
- Antihistamines
- Topical glucocorticosteroids
Severe Cases
- Systemic prednisolone may be considered if the disease is extensive and pruritus does not resolve.
Spontaneous Resolution
- The disease typically resolves within 4–6 weeks, independent of delivery.
Prognosis and Fetal Risks
Prognosis
- PEP is a self-limiting disorder.
- Does not affect the prognosis for the fetus or the pregnant patient.
Recurrence
- Rare, usually occurs only in first pregnancies.
Pemphigoid Gestationis (PG)
Definition and Epidemiology
- Also known as herpes gestationis.
- Rare self-limited pregnancy-associated bullous autoimmune disease.
- Incidence: Approximately 1 in 2000 to 1 in 60,000 pregnancies.
- Typically occurs in late third trimester but can develop at any time during pregnancy or immediately postpartum.
- Recent reports indicate its occurrence in egg donation pregnancies and rarely in association with trophoblastic tumors.
Pathophysiology and Clinical Characteristics
Pathogenesis
- Similar to bullous pemphigoid with autoantibodies (IgG1 subclass) against bullous pemphigoid antigen 180 (BP180).
- Autoimmunity primarily targets placental proteins, leading to cross-reaction with skin BP180-2 proteins.
- Results in complement activation, eosinophil recruitment, and blister formation at the dermoepidermal junction.
Clinical Presentation
- Initial severe pruritus followed by polymorphic inflammatory skin lesions.
- Erythematous urticarial papules and plaques, often periumbilical, spreading to the abdomen, extremities, and mucosal membranes.
- Progression to tense blisters resembling bullous pemphigoid.
Diagnostic Workup
Diagnosis
- Based on clinical presentation.
- Direct immunofluorescence (DIF) shows linear C3 and/or IgG deposits along the dermo-epidermal junction.
- Histology is nonspecific; biopsy may be performed to exclude other dermatoses.
- Complement-binding tests like ELISA for circulating IgG antibodies against BP180 may be used.
Treatment
First-line Treatments
- High-potency topical glucocorticosteroids and antihistamines to reduce pruritus and prevent blister formation.
- Non-fluorinated topical glucocorticosteroids preferred for less systemic absorption and fewer side effects.
Second-line Treatments
- Short courses of systemic prednisolone if topical treatments are inadequate.
- Other agents like calcineurin inhibitors, intravenous immunoglobulins, dapsone, and azathioprine are considered if refractory to steroids.
- Rituximab before conception may prevent recurrence in subsequent pregnancies.
Prognosis and Fetal Risks
Fetal Prognosis
- Relatively good, but risks include preterm labor and intrauterine growth retardation.
- Risks are likely linked to disease severity rather than treatment.
Association with Other Autoimmune Disorders
- Increased risk of autoimmune disorders in pregnant patients, especially Graves disease.
Recurrence in Subsequent Pregnancies
- Common, with earlier onset and more severe forms reported.
Intrahepatic Cholestasis in Pregnancy (ICP)
Definition and Epidemiology
- Liver disorder unique to pregnancy.
- Incidence: 0.3–5.6%, with ethnic, geographic, and seasonal variations.
- Striking geographic variation, with higher incidence in certain populations, such as Araucanian Indians (up to 28%).
- Mutations of ABCB4 (MDR3) implicated in biliary secretion of phospholipids may contribute to ICP.
- Associated diseases: gallstones, hepatitis C infection, preeclampsia, and gestational diabetes.
- Characterized by inability to excrete bile salts from the liver, leading to increased serum bile acid concentration and pruritus.
- Typically occurs in the second and third trimesters (>30th week), but earlier onset has been reported sporadically.
Pathophysiology and Clinical Characteristics
Reversible Cholestasis
- Due to impaired excretion of bile salts from the liver.
- Increased serum bile acid concentration leads to pruritus, possibly due to increased availability of brain opiate receptors.
- Negative impact on fetal prognosis.
Etiopathogenetic Factors
- Genetic alterations in hepatobiliary transport proteins.
- Hormonal influences, particularly estrogen levels.
- Environmental factors like seasonal variability and diet.
- Potential role of gut microbiota alterations and long-term therapy with vaginal progesterone preparations.
Clinical Triad
- Severe pruritus, jaundice starting 2–4 weeks after pruritus onset, and elevated bile acids.
- Elevated serum bile acids (>10 μmol/l) and abnormal liver function, mainly serum transaminases.
- Jaundice is not always present, reported in only about 10% of patients.
- Pruritus typically begins on palms and soles, and may become generalized, without primary skin lesions.
- Pruritus may worsen with pregnancy progression, other symptoms include steatorrhea and dark urine.
- Steatorrhea may lead to vitamin K deficiency, requiring careful monitoring of prothrombin time.
Diagnostic Workup
Diagnosis
- Based on clinical presentation and laboratory tests.
- Elevated levels of total serum bile acids are a key indicator.
- Liver function tests may show elevated transaminases.
- Other tests may be performed to rule out associated diseases, such as hepatitis C infection.
Exclusion of Other Conditions
- Exclusion of other cholestatic and hepatic diseases.
- Serum bile acid levels >10 μmol/l.
- Mild elevations in liver transaminases.
- Ultrasound and serologic tests to rule out other potential causes.
- Diagnosis based on characteristic symptoms and increased total serum bile acid levels.
Treatment
First-line Treatments
- Ursodeoxycholic acid (UDCA) is the mainstay of treatment, reducing serum bile acid levels and relieving pruritus.
- Close monitoring of maternal and fetal well-being is essential.
- Delivery may be considered if maternal or fetal complications arise or if the condition worsens despite treatment.
Spontaneous Resolution
- The disease typically resolves within 6 weeks after delivery.
Additional Treatments
- Primary goal: Reduce serum bile acid levels to alleviate symptoms and decrease fetal risks.
- First-line treatment: Ursodeoxycholic acid (UDCA) 15 mg/kg/day or 1 g daily is administered until delivery.
- Consideration of rifampicin synergistic effect in severe cases (>100 µmol/l) if no improvement with UDCA alone.
- Elective delivery after gestation week 37, especially if bile acid concentrations are >100 mmol/l.
Prognosis and Fetal Risks
Prognosis
- Reversible condition with favorable prognosis for both mother and fetus with appropriate management.
- Risks include preterm birth, meconium-stained amniotic fluid, fetal distress, and stillbirth, particularly in severe cases or if untreated.
- Increased vigilance and regular monitoring are necessary to mitigate potential risks to both mother and baby.
Associated Fetal Complications
- Perinatal mortality, stillbirths, low birth weight, preterm birth, and fetal distress during labor.
General Considerations for Pharmacological Treatment of Chronic Pruritus During Pregnancy
Topical Treatment
- Glucocorticosteroids:
- First-line treatment for CP with inflammatory skin lesions.
- Commonly used: Low- or moderate-potency (e.g., methylprednisolone aceponate).
- Safe: No causal associations with pregnancy outcomes for low- or moderate-potency topical glucocorticosteroids.
- Caution: Excessive use of potent/very potent steroids (>300 g during pregnancy) may risk low birth weight.
- Calcineurin Inhibitors:
- Alternative if steroids are contraindicated/refused.
- Usage: Small areas only, max 5 g/day for 2–3 weeks or as needed.
Systemic Treatment
- Antihistamine Drugs:
- Early Pregnancy: First-generation H1 antihistamine chlorpheniramine (FDA pregnancy category B).
- From Second Trimester: Second-generation antihistamines like loratadine, cetirizine, levocetirizine (FDA pregnancy category B), and fexofenadine (FDA pregnancy category C).
- Phototherapy:
- Narrowband UVB is safe, especially in early pregnancy.
- Supplement folate to reduce neural tube defect risk.
- Prevent melasma: Facial covering advised.
- Glucocorticosteroids:
- Short-term systemic treatment for severe pruritus.
- Prednisolone is preferred, with caution, especially in the first trimester.
- Other Immunosuppressive Agents:
- Cyclosporine (FDA pregnancy category C) or azathioprine (FDA pregnancy category D) for non-responsive cases.
- Monitor maternal blood pressure and renal function with cyclosporine use.
- Biologics and Small Molecules:
- Omalizumab (FDA pregnancy category B) and dupilumab for refractory cases (limited safety data).
- Dupilumab use should be postponed until more safety data is available.
Pruritus in Pregnancy (Not Specific to Pregnancy)
General Causes of Itching in Pregnancy
- Dry skin (most common cause of generalized itch)
- Renal abnormalities
- Hepatic abnormalities
- Thyroid abnormalities
- Iron deficiency anemia
- Malignancy
- Rheumatic diseases
- Drug reactions
- Diabetes
- Infestations
- Neurologic disorders
- Primary psychiatric disorders
- Systemic infections (e.g., hepatitis, HIV)
Specific Conditions
Atopic Dermatitis
- Chronic inflammatory skin disease
- Associated with skin barrier impairment
- Eczematous lesions and itching
- History of atopy common
Prurigo Nodularis
- Chronic inflammatory skin disease
- Very itchy nodular lesions
- Constant pruritus and scratching
- Unknown pathophysiology
Psoriasis
- Common, long-lasting inflammatory skin disease
- Affects approximately 2% of people
- Red, thick, scaling plaques
- Historically thought not to cause significant itching
- Pruritus commonly affects legs, hands, body, back, and scalp
Notalgia Paresthetica
- Chronic pruritus on the back
- Located lateral to the thoracic spine, interscapular, and paravertebral areas
- Affects women more than men
- Unclear pathogenesis
Other Causes
- Pigmented contact dermatitis
- Pityrosporum folliculitis
- Parapsoriasis
- Neurodermatitis
- Primitive cutaneous amyloidosis
Vulvovaginal Itching
Multiple Etiologies
- Lichen planus
- Atopic and irritant contact dermatitis
- Lichen simplex chronicus
- Lichen sclerosis
- Psoriasis
Vulvovaginal Candidiasis
- Common due to increased estrogen levels
- Usually caused by Candida albicans
Parasitic Infestations
- Pediculosis pubis
- Scabies
Lichenoid Vulvar Diseases
Lichen Sclerosis
- Involves vaginal, perineal, and perianal skin
- Rarely seen during pregnancy
Lichen Planus
- Autoimmune disorder
- Causes pain and intense pruritus (affects approximately 1% of the population)
Lichen Simplex Chronicus
- Eczematoid disorder
- Results in repetitive itch-scratch cycle
Pruritus of Unknown Origin
- Affects 61% of pregnant women
References
#Addressing Chronic Pruritus in Pregnancy #Pruritus in Pregnancy